|
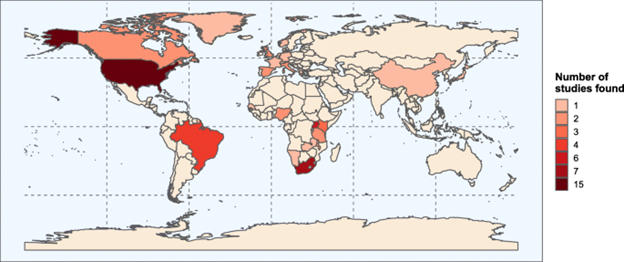
High blood pressure is more common among people living with HIV than HIV-negative people in North America, but the reverse is true in Africa and Asia, according to a review of the evidence led by Manicaland Centre researchers. In this post, Manicaland Centre postgraduate researcher Katherine Davis explains the findings. High blood pressure is among the leading causes of death and disability globally. With improved HIV treatment, people living with HIV are beginning to age and develop chronic conditions, including high blood pressure. Nevertheless, it has been unclear whether people living with HIV are more likely to have high blood pressure than HIV-negative people. To bridge this data gap, we systematically reviewed the results from 59 studies of HIV and high blood pressure in adults. We found that high blood pressure is less common among people living with HIV than HIV-negative people globally. However, there are substantial differences by region. In North America, high blood pressure is more common among people living with HIV than HIV-negative people. By contrast, in Africa and Asia high blood pressure is more common among HIV-negative people than people living with HIV. Lastly, in South America and Europe, there isn’t evidence of a difference between people living with HIV and HIV-negative people. It is interesting to consider why we see these differences between regions. One possible explanation relates to diversity in the amount of time that people are exposed to both HIV and HIV treatment. For example, in North America access to HIV treatment and survival of people living with HIV remains better than in Africa and Asia. This may mean that more people have long term exposure to HIV and HIV treatment in North America, which could increase their risk of high blood pressure. Whatever the explanation for the differences, there are important policy ramifications to our findings. In areas with greater burdens of high blood pressure among people living with HIV, targeted prevention of high blood pressure needs to be scaled up. Promoting healthy diets, exercise, avoidance of tobacco, and reduction of alcohol consumption to people living with HIV could have a large impact. Ensuring that people living with HIV can easily access testing and treatment for high blood pressure through integrated, friendly services will also be key. In regions where the burden of high blood pressure is lower and deaths related to AIDS remain common, boosting access to HIV care must continue to be a priority. However, policymakers should also recognise that if access is successfully increased, the population of people living with HIV will age and it is likely that the burden of high blood pressure among people living with HIV will increase. Acting now to bolster prevention and train community healthcare workers in managing high blood pressure could be useful preparation for this. In addition to consequences for policy, our study also has implications for research. Despite a systematic search, we could only find two studies exploring the link between HIV and high blood pressure in Asia. New studies across a range of Asian countries are needed to give us a clearer picture of the relationship between HIV and high blood pressure in the region. With the evidence available today, it is clear that the burden of high blood pressure in people living with HIV varies by region. Our results emphasise the need for expanded prevention and care for high blood pressure, which is tailored to local contexts. Read the systematic review: Association between HIV infection and hypertension: a global systematic review and meta-analysis of cross-sectional studies. Author Katherine is a postgraduate researcher on the Wellcome Trust PhD Programme in Epidemiology, Evolution and Control of Infectious Diseases at Imperial College London. Her work with the Manicaland Centre focuses on non-communicable diseases and mental health. Email: [email protected] Twitter: @kd_katdavis Comments are closed.
|
Archives
December 2023
Categories |


 RSS Feed
RSS Feed