HIV Rapid Tests Study
|
There is growing evidence that large numbers of people in sub-Saharan Africa may be receiving incorrect information about their HIV status due to errors in HIV rapid test results (misclassification errors) obtained from HIV testing conducted as part of routine health services. This may lead to delayed or incorrect initiation onto antiretroviral therapy which, in turn, would have negative consequences for health, survival, and onward transmission of HIV infection.
In this study, we conduct an in-depth investigation into the causes of misclassification errors by adapting and extending the comparison of results from health-worker-administered HIV rapid tests with results from carefully-controlled ELISA tests conducted in a central laboratory in an already planned and funded round of national HIV surveillance in Zimbabwe. Using data from this investigation, we will assess the epidemiological and health service impacts of misclassification errors using a mathematical model. Findings from these investigations then will be discussed with key stakeholders to establish acceptability thresholds and technological and quality assurance solutions considered necessary to reduce misclassification errors. |
|
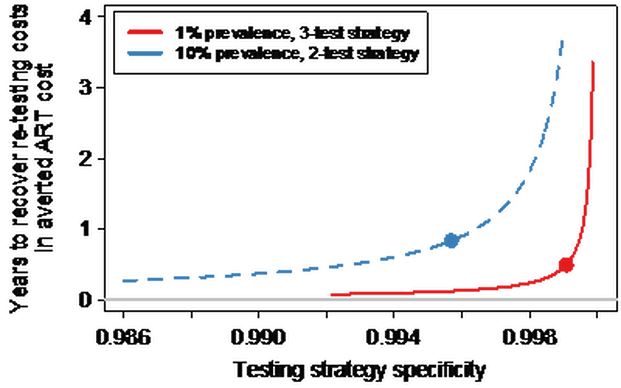
Figure 1: The number of years after which cost of re-testing is surpassed by the expected cost of providing ART to HIV-negative adults, for increasing specificity of primary testing strategy. It assumes re-testing costs are the same as primary HIV testing costs. The dots on graph illustrate testing strategy specificity for baseline scenario described in the full paper which can be found here. |